Globally, it’s estimated that over 19 million people are diagnosed with cancer each year, and these statistics continue to rise with 1 in 2 of us expected to develop some form of cancer within our lifetime, it’s estimated there will be 28 million new cases annually by 2040. The relentless pursuit of conquering this devastating disease remains one of humanities biggest challenges.
Cancer is a complex group of diseases characterized by the uncontrolled growth and spread of abnormal cells, a series of genetic mutations that accumulate over time disrupting the normal regulation of cell growth and division. Traditionally, cancer is detected utilising various diagnostic methods depending on the suspected disease as methods may vary and some cancers remain undetectable to a range of diagnostic tools. A combination of Imaging (X-Ray, CT, MRI & Ultrasound), biopsy, blood counts and clinical examinations are used to detect cancer and the initial detection can be time consuming and challenging often requiring multiple experts to examine the results. As we enter the era of Artificial Intelligence, there is untapped potential to unearth groundbreaking new detection methods, treatment plans and lifesaving technology.
integration of AI
Integration of artificial intelligence has the scope to change the landscape of cancer research and in recent years, the fusion of cutting-edge technologies and AI has propelled this medical field into a new era, enabling scientists and healthcare professionals to unravel complex biological mysteries, accelerate drug discovery, and personalise treatment strategies. The synergy between AI and cancer research has not only enhanced the speed and efficiency of data analysis but has also opened unprecedented avenues for understanding the intricacies of the disease at a molecular level. As we navigate this intricate intersection of technology and medicine, the partnership between AI and cancer research holds the promise of paving a future where innovative solutions and personalised therapies lead the charge against cancer’s devastating effects.
Artificial Intelligence (AI) has shown great promise in advancing cancer research, enhancing various aspects of diagnosis, treatment, and overall understanding of the disease.
Importance of early detection
Early Detection has been recognised as a key priority by the World Health Organisation (WHO) and the International Alliance for Cancer Early Detection (ACED) and an early diagnosis is crucial in the battle against cancer, and significantly improves the patient prognosis. An essential approach involves screening high risk or genetically predisposed patients that show no symptoms, and investigating patients who present symptoms swiftly and efficiently. Machine learning, whereby computers learn complex data patterns to make predictions, has the potential to revolutionise early cancer diagnosis. Due to its invasive nature, the early detection often means that the cancer is more localised meaning it’s more amenable to surgical removal or targeted therapies, treatments may be less aggressive and more treatment options may be available. Treatments at an early stage greatly increase the changes of a cure, or long-term management of the cancer all of these contribute to a better quality of life for the patient. The use of AI algorithms can analyse medical imaging data, such as mammograms, CT scans, and MRIs, to detect subtle patterns and anomalies that may indicate the presence of cancer at an early stage. Machine learning models can help pathologists in analysing pathology slides, improving the accuracy and speed of cancer diagnosis.
Genomic research
Genomic cancer research is the study of DNA sequences, and gene expression differences between the tumour cells and the patients normal host cells and most cancers are caused by acquired genomic variants. The use of AI in analysing genomic and molecular data to identify specific genetic mutations or biomarkers associated with cancer can aid oncologists in developing precision medicines and personalised treatment strategies for individual patients. Predictive modelling can help oncologists anticipate how a patient is likely to respond to certain treatments, optimising the use of therapeutic strategies.
Drug discovery and clinic trials
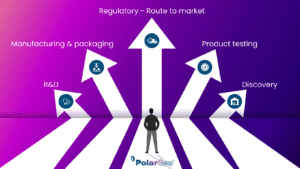
Drug discovery and development is a costly and time-consuming process. AI can accelerate drug discovery by analysing vast datasets to identify potential drug candidates and predict their effectiveness. This can significantly reduce the time and cost involved in bringing new cancer therapies to market. Virtual screening and in-silico modelling (computer screening) can enable researchers to simulate and predict the interactions between drugs and cancer cells, aiding in the development of more targeted and effective treatments. The drug development itself can take years to perfect, there is no average timeframe to bring to market it may take 10-15 years to complete before it even reaches the clinical trial stage. Once at the clinical trial stage there are 4 phases, each with a different purpose;
Phase 1 – Safety (10-15 Patients)
Phase 2 – Effectiveness (<100 Patients)
Phase 3 – Comparison (100’s Patients)
Phase 4 – Approval (1000’s Patients)
AI can help identify suitable candidates for clinical trials by analysing patient data and matching individuals with specific characteristics to the appropriate trials. This can lead to a more efficient and inclusive trial recruitment processes. Predictive modelling can assist in forecasting patient responses to experimental treatments, aiding in trial design and execution.

radiation therapy
Radiation Therapy is a commonly used to treat a wide variety of cancers. Radio therapy works by killing cancer cells or slowing their progression by damaging their DNA, the aim of the treatment is to damage the cells beyond repair killing them entirely and preventing them dividing further, the cells are then broken down and removed by the body. However, as well as attacking and damaging the cancerous cells, radio therapy can also attack and harm the healthy cells and this is why patients experience the side effects we associate with the treatment, such as hair loss, fatigue, nausea an vomiting headaches among others. AI can optimise the planning of radiation therapy by precisely targeting cancerous cells while minimising damage to surrounding healthy tissues, previously physicians manually outline the organs and tissue they wish to protect on scans ahead of radiation, the process when completed by AI can be completed 2.5x faster than manually and with higher levels of accuracy, this enhances the effectiveness of treatment and reduces damage to the healthy tissue reducing side effects.

data intergration
Data Integration and Analysis is integral to advancing the research and treatment of cancer, though the global data available is incredibly vast and AI has the potential to integrate and analyse diverse data sources, including electronic health records, imaging data, peripheral blood pathology slides and genetic information in great depth and speed, to provide a comprehensive understanding of cancer. This holistic view can lead to new insights and correlations aiding the prevention of the disease and not just the treatment. Data analysis can also be utilised for patient monitoring, AI-based tools can continuously monitor patient data, helping in the early detection of disease recurrence, providing real-time insights into a patient’s health status.
While these advancements are promising, it’s important to note that challenges, such as data privacy concerns, ethical considerations, and the need for rigorous validation, still exist. Collaborations between researchers, clinicians, and technology experts are crucial to realising the full potential of AI in cancer research.
Read More from PolarSeal

How AI could advance the healthcare industry?
Artificial Intelligence, commonly referred to as ‘AI’ is a rapidly growing technology advancement whereby technology, i.e. computers, machines and devices are programmed with the ability
What to consider when classifying a medical device
Medical device classification is a regulatory process that categorizes medical devices into different classes based on their intended use, risks, and other relevant factors. The

7 Types of Diagnostic Products & Wearable Diagnostic Devices Important in the Personal Healthcare Industry
The medical industry is constantly evolving, and new diagnostic products and wearable diagnostic devices are key to keeping healthcare teams ahead of the curve and